
An alternative perspective on mental health and addiction.
Contents
Forward
What if Doctor is Wrong? : The Research and Practices
Chapter One: Basic Instinct
Chapter 2: The Importance of Words (Part 1)
Chapter 2: The Importance of Words (Part 2)
Chapter 2: Citations, Bibliography and additional sources
Chapter 3: But I Don't Have Trauma

Many people aren’t aware they have trauma because it’s generally believed to only be the result of a once off life threatening situation.
So let’s talk more about what trauma is and how it works.

What is trauma?
A person is left with trauma from the feeling of being isolated, overwhelmed and unable to manage a situation during a high stress experience.
Being traumatized has more to do with how a person perceived and experienced the situation than the incident or situation itself.
This is how some people can be in the exact same situation and one can end up with trauma and one not.
In other words, the result of trauma is more dependent on how capable and supported a person felt during the circumstances than the situation itself.
The degree of trauma a person is left with also depends on how capable and/or supported the person felt during the situation.
For example:
Two people are out fishing together.
One person can swim and one can’t.
They’re relatively close to the shoreline when the boat capsizes. They hear a sea gull cry overhead. They see the painted green wooden slats of the bottom of the boat, capsized in the near distance.
The person who can swim laughs at the situation, takes hold of the person who can’t swim and easily helps them to shore.
The person who can’t swim remembers to wear a lifejacket or decides to learn to swim before they get back onto a boat again.
When they hear a sea gull cry or see a green boat they may remember the incident with some objectivity.
The response of the mind is rational and healthy.
In the second version of the story the one person can’t swim and their friend, who can swim, is killed by a shark.
The person who can’t swim is left alone, struggling to stay afloat. They see the bloodied water and believe they are about to die as well. They are terrified and overwhelmed.
At this point the mind will disconnect (dissociate) from their emotions and conscious thoughts, so that the person is able to keep moving physically.
In order for them to survive.
In this state of dissociation the struggling person manages to grab onto the green wooden bottom of the capsized boat.
Some hours later, a passing ship rescues them.
But the event is not fully processed by the mind, in this second example, because of the dissociation / disconnect.
This is why the person is left with trauma in the form of Post Traumatic Stress Disorder (PTSD, which I’ll refer to as PTSR - Post Traumatic Stress Reaction moving forward, in line with the perspective of this conversation).
This is what trauma is.
Trauma is unresolved or mentally “un-processed” events, and information, because of an internal “disconnect” that happens between the mind, the feelings and the external environment associated with the situation…
to facilitate survival.
Trauma recovery focuses on helping a person re-experience the situation in a safe, supported space in order to help the mind process the event properly.

What happens when an event has not been fully processed by the brain due to trauma
Since the mind wasn’t really “conscious”, because of the dissociation, it didn’t have the opportunity to file the information associated with the high stress situation into relevant “folders”.
The brain simply lumped everything associated with the event into a folder marked “Danger”.
Randomly and unspecifically.
If experiences are processed in a healthy way, the brain will file information into relevant “folders” in the brain, to refer to in the future, that it deems useful for survival. And it’ll discard the information it deems unnecessary over time.
Remembering that this is an oversimplification for illustration purposes.
For this basic explanation, imagine there are different folders in the brain that are marked with category names like:
“Tools”, “Communication” etc. and among these is a folder categorized as “Danger”.
As a person goes through life, and learns, the brain adds things to the different folders for the person to refer to when they’re needed. It adds the things it deems dangerous to the folder marked “Danger” in order to avoid harmful experiences, or to not repeat them, and to keep a person safe.
If a child tries to touch a candle flame and burns their finger, for example, the brain will add “candle”, “fire” and maybe “hot”, “burn”, “don’t touch”, and such things, to the folder categorised as “Danger”.
The child will learn that a candle is not dangerous, but a lit candle is dangerous. If they are introduced to this information consciously.
This happens so the person may avoid getting hurt again and is a part of the natural mechanism of survival mentioned in Chapter One (the Fight / Flight Stress Response).
Our animal instinct to survive.

Let’s return to the above example of the person who is left traumatized by an unprocessed event. The boat capsizing and the shark attack.
Because the brain didn’t have the opportunity to process this event properly, everything that was a part of (or vaguely related to) the situation will simply be dumped into the folder marked “Danger”.
The brain hasn’t had a chance to sift through the information properly to “learn” what was actually dangerous in the situation.
i.e. That the person was on a boat but couldn’t swim and didn’t have a life jacket on, for example (dangerous). Or that the red in the water was blood because of the shark bite (sharks can be dangerous but you only find them in the ocean). Or that the cries of seagulls were audible because the person was near the ocean (sea gulls are not dangerous).
But the brain hasn’t had the opportunity to do this.
Now, even the cry of a gull, the sound of crashing waves, making red jelly with their child (the red water) or seeing the hull of a green boat will trigger a warning signal in the Amygdala (directly related to the folder marked Danger) that there is an imminent threat in the person’s current environment.
Even if there isn’t.
To remind you, from Chapter 1, the Amygdala controls the Fight/Flight Stress Reaction when a threat is perceived, to kick the person into the stress response so that they are able to react and find safety.
Now, because the brain has not had the opportunity to sift through the information and the cry of a seagull has been added to the folder marked "Danger", hearing the cry of a seagull in a present situation “triggers” a danger signal in the Amygdala, which sends a signal to the Hippocampus to set off the Fight/Flight Response via the nervous system.
This is not just a mental reaction.

After the brain’s reaction, there is also a physical reaction to the “trigger” as the Fight/Flight Stress Response kicks into gear. Heart rate will increase, adrenalin will be released into the body, etc. to enable the person to fight or flee.
This is a “trigger” and a “flashback” and how these work in practice.
Something from an unprocessed event in a person’s history incorrectly alerts the brain that there is danger in the present moment.
trigger
n. a stimulus that elicits a reaction. For example, an event could be a trigger for a memory of a past experience and an accompanying state of emotional arousal.
vb. to act as a trigger. [9]
flashback
n.
- the reliving of a traumatic event … Memories may be triggered by words, sounds, smells, or scenes that are reminiscent of the original trauma (as in a backfiring car triggering a flashback to being in combat). [9]
What happens, when a person is triggered and is having a flashback, is that there’s also a strong sense of being back in the situation.
The perception and thinking of the person change, accordingly, and are often out of sync with the present moment.
It sounds simple, doesn’t it?
But there is more than one type of trauma and this is where things become a little less obvious and easy to understand.
So let’s talk more about the types of trauma and the reasons a person may have them.
Because C-PTSD C-PTSR (Complex Post Traumatic Disorder Reaction) was only first acknowledged in 1992, if you remember this from Perfect - Chapter 2: The Importance of Words.

What is C-PTSD / C-PTSR?
While Post Traumatic Stress Reaction (PTSD / PTSR) is caused by a once off high stress / life threatening incident (or witnessing or hearing about such an incident), C-PTSR occurs when people are exposed to a threat of harm or injury (micro traumas), or even a feeling that they are not safe, over an extended period of time.
The types of trauma that often result in C-PTSR are:
Developmental Trauma, Hereditary Trauma and Multi-generational Trauma. As well as trauma from abusive/dysfunctional relationships (Relational trauma).
Although we like to separate these circumstances, and classify the resultant trauma with different names, they’re all the same thing really. The types of trauma listed above all happen to people in extended circumstances (commonly family and relationship environments) and, thus, result in C-PTSR.
So again… for the purposes of this conversation, let’s just keep things simple and say it really doesn’t matter what type of trauma we’re talking about, as long as we’re aware that there are two main sets of reactions that result from all of them.
The reactions of PTSR and C-PTSR.
Since the Amygdala sets off the Fight/Flight Stress Response, when it perceives a threat in the present moment as one of its key roles in the survival mechanism, it’s easy to understand how people with PTSR and C-PTSR could be incorrectly triggered into the same Fight/Flight response when they have a “flashback”.
When you understand more about how trauma works.
Having a “flashback” (i.e. being unexpectedly cast back into the traumatic event emotionally and psychologically, as well as actively being pushed into the Fight/Flight Stress Response because of this) will make people volatile, violent, unpredictable and severely emotionally dysregulated.
If children and loved ones are exposed to these reactions over extended periods of time they will end up with C-PTSR and PTSR as well.
This is how Multi-generational and Hereditary trauma is passed on.

My eating disorder, for example, is kicked off if current circumstances mimic the primary trauma that set this addictive behaviour in motion.
The behaviour was learned from family members who also have disordered eating.
Remembering that, when a person is in a “flashback”, they are subconsciously thrown back into the time of the circumstances that left them traumatized:
When a trigger of a primary trauma sent me into the fight/flight reaction (anxiety or depression were my Fight/Flight reactions related to the primary cause of my ED), I would mimic the behaviour of the primary care-giver who had the same eating disorder, in a subconscious effort to get them to accept and rescue me.
To subconsciously try to change the outcome of the primary trauma.
In order to find safety again.

I found that I could apply this exact formula to my substance abuse as well.
My addiction and addictive behaviours were a completely logical, albeit unhealthy, learned response to my primary traumas, early childhood environment and family.
My anxiety, depression, schizophrenia, bipolar or whatever the doctor at the time chose to label it…
Was only PTSR and C-PTSR.
By doing some years of deep trauma recovery, my addiction and addictive behaviours completely (and seemingly miraculously) disappeared.
And so did my mental and emotional dysregulation.
It isn’t a miracle. Or even surprising.
When I processed the trauma the triggers abated and (along with the information gleaned on why I was struggling) I was no longer dysregulated. Consequently, I no longer felt the desire or need to use substances or behaviours to avoid the present.
No more medication. No more therapists. No more support groups. No more programs required to stay regulated or sober.
My mental health and addiction challenges simply vanished in full.

Some people are going to stubbornly insist on the Biological approach, or Disease model, as the reason people have these kinds of reactions and maladjusted behaviours in their attempts to self soothe/find safety again. (These are not attempts to “self medicate” as we like to insist they are).
My answer to the biological/disease perspectives would be this:
While exposure to long term high stress situations does impact the physical structure of the brain (long term exposure to trauma shrinks/enlarges different areas of the brain depending on age), which will make the brain hypersensitive (or less sensitive) to stress and more (or less) mentally and emotionally responsive, this is not what causes a person’s mental health or addiction challenges initially in my experience.
Changes in physical structure in the brain are also a result of trauma. Scientifically proven fact now.
Parents with unresolved PTSR and C-PTSR will pass this on to the children in the environment via their own reactions, via their traumatized perspectives (e.g. “the world is not safe”) and because of the children’s nervous systems physically syncing with the nervous systems of the adults around them.
The children also learn the maladjusted coping mechanisms that their parents may have adopted in order to survive… by rote.
Because this is how children learn. By instinctively mimicking the adults around them to win the parents over. To get the parents to accept and protect them.
In order to survive.
Yes. I am saying that anxiety and depression are passed on environmentally and possibly learned by rote. And so is addiction.
It’s a big statement and I’m prepared to openly discuss why I now believe this, here on Hive. Please feel free to ask questions and comment to keep everything on this feed for those who may need it to refer to.

Moving back to this conversation, it’s easier to understand what I am trying to say by adding the word “abuse” to the conversation.
I hope the word “abuse” doesn’t trigger you into leaving this conversation because this is for illustration purposes and most childhood trauma is passed on completely accidentally by loving, caring parents.
So stay with me, please, because this is important for you and your children.
The addition of this word is easier to understand if we simply list the behaviours of PTSR and C-PTSR and compare them to behaviours that are considered to be emotionally and psychologically abusive.
But before we do, I quickly want to note the other difference between PTSR and C-PTSR.

PTSR triggers and subsequent flashbacks will be visual, sensory or auditory.
It is quite easy to know where a person with PTSR’s disproportionate reactions to the current circumstances may come from.
C-PTSR triggers, however, are barely noticeable and the flashbacks are more “feeling” orientated (commonly called “emotional flashbacks”).
The triggers for C-PTSR are much harder to see, or understand, because the trauma happened over an extended period of time and was “normalized”. This will often leave a person suffering with C-PTSD confused as to why they may be reacting strongly at times.
Triggers for C-PTSD flashbacks are so subtle that a person with C-PTSR will often not know they’ve been triggered into the Fight/Flight Reaction at all.
Now let’s have a look at PTSR, and C-PTSR and what perspective, reactions and behaviours are exhibited by people suffering with these first.

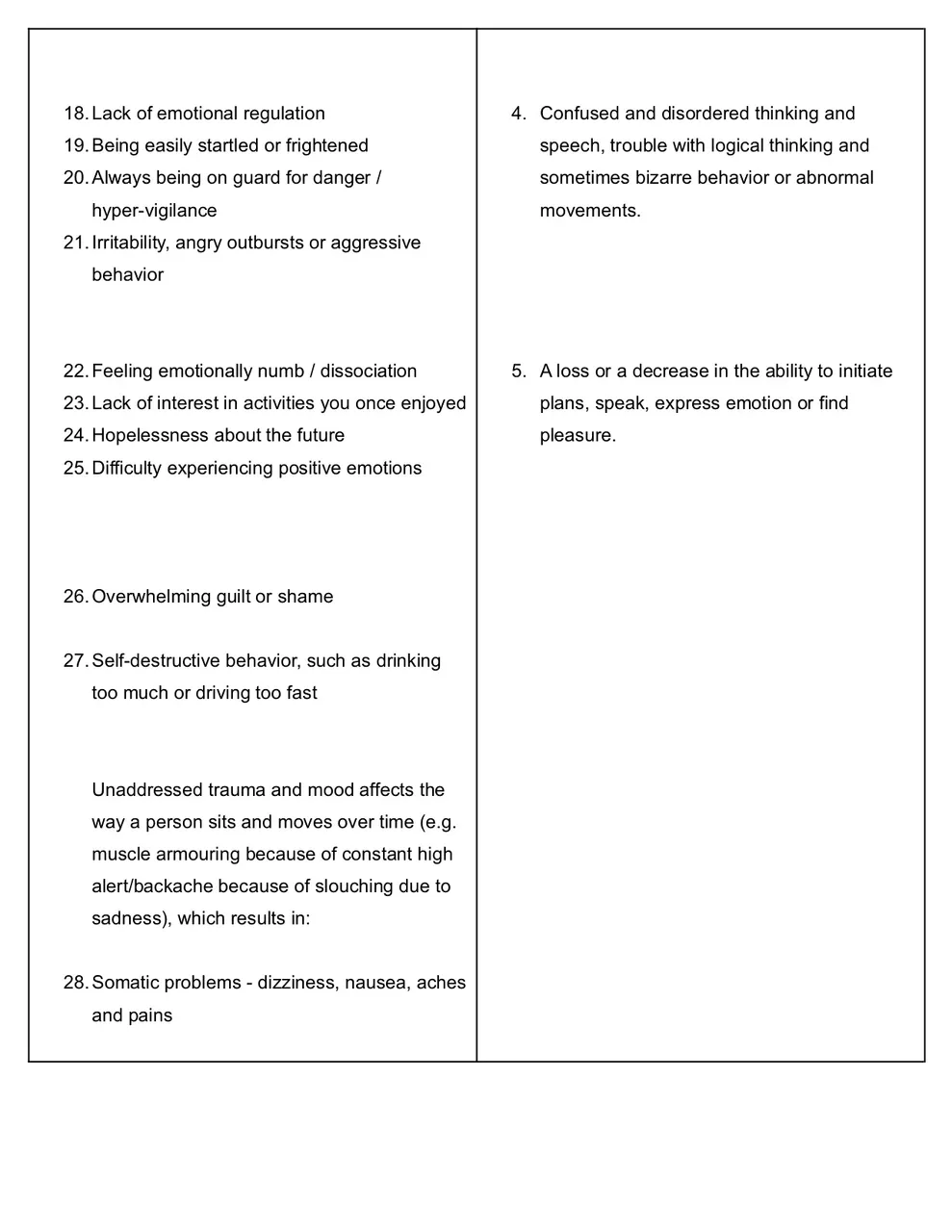
POST TRAUMATIC STRESS REACTIONS (PTSR)
[10]
- Recurrent, unwanted distressing memories of the traumatic event
- Reliving the traumatic event as if it were happening again (flashbacks)
- Upsetting dreams or nightmares about the traumatic event
- Severe emotional distress or physical reactions to something that reminds you of the traumatic event
- Trying to avoid thinking or talking about the traumatic event
- Avoiding places, activities or people that remind you of the traumatic event
- Negative thoughts about yourself, other people or the world
- Hopelessness about the future
- Memory problems, including not remembering important aspects of the traumatic event
- Somatic problems - dizziness, nausea, aches and pains
- Difficulty maintaining close relationships
- Feeling detached from family and friends
- Lack of interest in activities you once enjoyed
- Difficulty experiencing positive emotions
- Feeling emotionally numb / dissociation
- Being easily startled or frightened
- Always being on guard for danger / hyper-vigilance
- Self-destructive behavior, such as drinking too much or driving too fast
- Trouble sleeping
- Trouble concentrating
- Irritability, angry outbursts or aggressive behavior
- Overwhelming guilt or shame
For children (but adults actually do this as well when they are “acting out" on their trauma and addictions):
- Re-enacting the traumatic event or aspects of the traumatic event
- Frightening dreams that may or may not include aspects of the traumatic event [10]

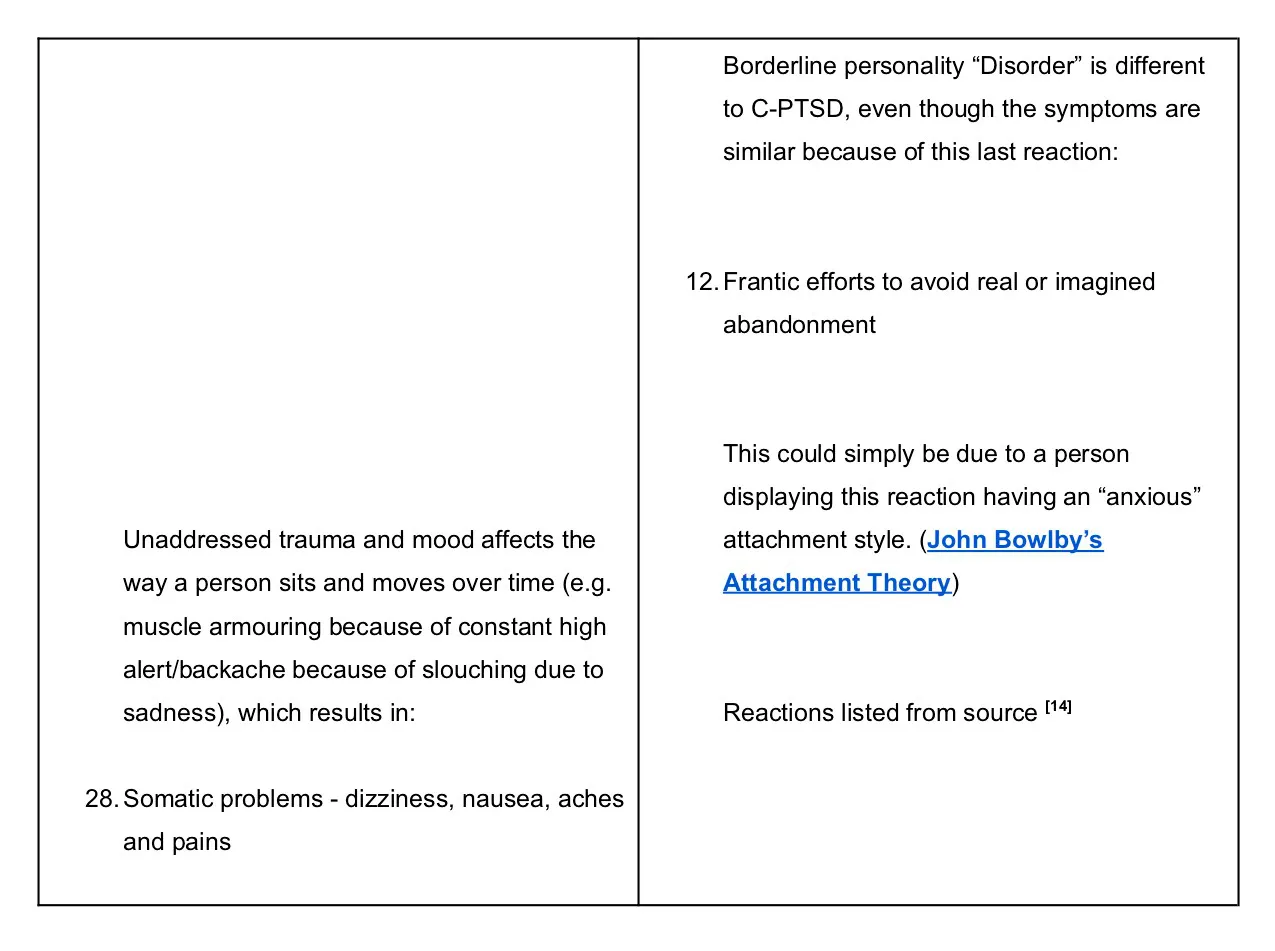
“Symptoms” of COMPLEX-POST TRAUMATIC STRESS (C-PTSR)
[11]
People with C-PTSR typically have the above PTSR symptoms along with additional symptoms (“emotional flashbacks” [added by me]), including:
- Lack of emotional regulation
This refers to having uncontrollable feelings, such as explosive anger or ongoing sadness.
- Changes in consciousness
This can include forgetting the traumatic event or feeling detached from your emotions or body, which is also called dissociation (derealisation, etc.).
- Negative self-perception
You may feel guilt or shame, to the point that you feel completely different from other people (every addict in recovery).
- Difficulty with relationships
You might find yourself avoiding relationships with other people out of mistrust or a feeling of not knowing how to interact with others. On the other hand, some might seek relationships with people who harm them because it feels familiar.
- Distorted perception of abuser
This includes becoming preoccupied with the relationship between you and your abuser. It can also include preoccupation with revenge or giving your abuser complete power over your life (can include denial about parents’ “abusive” behaviour, their personal challenges and the dysfunction in the family system [Added by me]).
- Loss of systems of meanings
Systems of meaning refer to your religion or beliefs about the world. For example, you might lose faith in some long-held beliefs you had or develop a strong sense of despair or hopelessness about the world. [11]
Simply because of the reactions that people with PTSR and C-PTSR have, and because of how addiction makes people unable to be fully present and capable when relating to other people, stressed and struggling parents can accidentally traumatize their children.
Because, as it turns out, the reaction of PTSR and C-PTSR, and the behaviours associated with them, are also listed as the reactions and behaviours that are considered to be the “emotional and psychological abuse” of adults and, specifically, children.
This is usually nobody’s fault and completely unintentional.
When a person is highly stressed, or is having a PTSR or C-PTSR flashback, they are not thinking clearly. They are not “themselves”.
They are acting on “animal instinct” as a result of the Fight/Flight Stress Response. The “reptile brain” has taken over and is driving the person to take action to “survive”.
Please be courageous and strong now, because this is important.
Let’s have a look at what the experts consider “emotional and psychological abuse” of children to be.

What is Considered Emotional and Psychological Abuse?
Psychological abuse of a child is often divided into nine categories: [12]
- Rejection: to reject a child, to push him away, to make him feel that he is useless or worthless, to undermine the value of his ideas or feelings, to refuse to help him.
- Scorn: to demean the child, to ridicule him, to humiliate him, to cause him to be ashamed, to criticize the child, to insult him.
- Terrorism: to threaten a child or someone who is dear to him with physical violence, abandonment or death, to threaten to destroy the child's possessions, to place him in chaotic or dangerous situations, to define strict and unreasonable expectations and to threaten him with punishment if he does not comply.
- Isolation: to physically or socially isolate a child, to limit his opportunities to socialize with others.
- Corruption or exploitation: to tolerate or encourage inappropriate or deviant behavior, to expose the child to antisocial role-models, to consider the child as a servant…(I would include forcing a child to take care of, or be responsible for, a struggling parent in this list item [added by me])
- The absence of emotional response: to show oneself as inattentive or indifferent towards the child, to ignore his emotional needs, to avoid visual contact, kisses or verbal communication with him, to never congratulate him.
Neglect: to ignore the health or educational needs of the child, to refuse or to neglect to apply the required treatment. (See: What is Child Neglect?)
- Exposure to domestic violence: to expose a child to violent words and acts between his parents.
The behavior of an emotionally abusive parent or caregiver does not support a child's healthy development and well-being-instead, it creates an environment of fear, hostility, or anxiety. A child is sensitive to the feeling, opinions, and actions of his or her parents.
- Showing a lack of regard for the child
This behavior often includes rejecting the child by:
-- Not showing affection.
-- Ignoring the child's presence and obvious needs.
--- Ignoring the child when he or she is in need of comfort.
-- Not calling the child by his or her name.
- Saying unkind things to the child
Emotionally abusive parents say things or convey feelings that can hurt a child deeply.
Common examples include:
- Making the child feel unwanted, perhaps by stating or implying that life would be easier without the child. For example, a parent may tell a child, "I wish you were never born" or complaining about costs of childcare etc.
- Ridiculing or belittling the child, such as saying, "You are stupid."
- Threatening the child with harsh punishment or even death.
- Continuous verbal abuse. [12]
People who are highly stressed or who are having PTSR and C-PTSR flashbacks will inflict a lot of what is listed above when they are triggered, COMPLETELY UNINTENTIONALLY, upon the people around them.
Interestingly enough, mental and psychological abuse is most commonly noted in families that are:
- having financial difficulties
- dealing with single parenthood
- experiencing (or have experienced) a divorce
- struggling with substance abuse issues [13]
There are some of what are considered the major life stressors listed here.
So, clearly, even stressed parenting can cause parents to act out “abusively” (unintentionally at times), which is possibly why stressed parenting has been clearly linked to early childhood trauma (Developmental and Relational Trauma).

When you understand how trauma works and look at the reactions of PTSR and C-PTSR, it would be almost impossible for a primary care-giver to remain stable and fully present, or to provide a consistently stable, “safe” environment for a child, if they are suffering from these.
Impossible, really.
A child would often be “neglected” while a parent with these challenges (or resultant addictions) had sudden, unexpected reactions, mood swings and shifts in perception. And possibly used addictive substances or behaviours in attempts to self soothe.
So even though the reactions and behaviours associated with trauma and its responses aren’t intentionally emotionally and psychologically abusive…
they are, in and of themselves, emotionally and psychologically abusive to those exposed to them…
according to the behaviours defined as emotional and psychological abuse.

"Symptoms" of Child Psychological Abuse
Symptoms of psychological abuse of a child may include:[12]
- Difficulties in school
- Eating disorders, resulting in weight loss or poor weight gain
- Emotional issues such as low self-esteem, depression, and anxiety
- Rebellious behavior
- Sleep disorders
- Vague physical complaints [12]
These look very similar to the “symptoms” of PTSR and C-PTSR, don’t they? (And ADHD and ADD as well…)

It doesn’t really matter what type of trauma it is, is what I’m trying to explain here.
It’s the fact that all of these types of trauma, which occur in extended situations or environments in which a child is not consistently supported emotionally / psychologically and is unable to extricate themselves from, cause PTSR and C-PTSR in the children in such environments as well.
PTSR and C-PTSR have a multitude and great variety of reactions, and subsequent behaviours, that I strongly believe are being misdiagnosed as some kind of mental illness or another.
Some people may now say that they have been through high stress experiences and their children are fine.
Allow me to clarify at this point, please.
It’s not the stressed parenting itself that causes the trauma.
It’s HOW the parent handles the stress.
Does the parent understand how trauma is passed on, or created, and know how to manage their own reactions and stay regulated, present and calm for the child?
Is the parent able to explain to the child that they are struggling with stress or unresolved trauma, to apologise if they react inappropriately and to let the child know that it is not the child’s fault?
Or is the parent still at the mercy of their own unconscious reptile brain, as their trauma/stress triggers them into the Fight/Flight reactions and makes them volatile, unstable and “unsafe” in the child’s experience?
Do the parents randomly explode or totally withdraw? Do they get anxious or depressed? Do they turn to alcohol or substances to try and alleviate their reactions? Are they unable to be consistently “present” and available for the child, to support the child in feeling as safe as possible?
Remembering that the child is going through their own development as they grow and attempt to navigate a greatly unknown (and sometimes intimidating) world that is new to them. And is trying to “individuate” successfully while they do this.
A vital time in a human being’s development and when much of the individual’s perception of the world, and themselves, is formed.

Regardless of whether it’s intentional or not, the reactions of PTSR and C-PTSR result in behaviours that are similar, or identical, to behaviours that are considered to be emotional and psychological abuse.
And the result of a child (or adult) being exposed to these reactions and behaviours, over time, will be trauma in the form of PTSR and C-PTSR as well. With the same reactions. And the same, or similar, addictive behaviours in attempts to self soothe.
If you combine this with the fact that children internalize their parents' bad moods or personal challenges (a well known fact in psychology), the adult child will be left, possibly permanently, with the belief that there is something inherently “wrong” with them. That they “are not good enough”. That they are “worthless”.
Or that they are, somehow, “different” to most people.
As adult, with C-PTSR, they may have a simple conversation, with someone seemingly random, and suddenly have a panic attack or sink into “depression”. (The “Freeze” response)
This is because the “emotional flashbacks” of C-PTSR have very subtle triggers and are very difficult to pinpoint. Most people with C-PTSR will not even know why they are being triggered. Or when they are being triggered.
They may even believe they have a mental “illness” or “disorder” because their mental and emotional dysregulation seems so irrational. And medical doctors tell them they have a “disorder” of some kind.
My reactions were completely rational and quite beautifully logical when I understood things better.
My so-called “symptoms” of the many misdiagnosed mental “disorders” were all emotional flashbacks from my C-PTSR.

The C-PTSR reactions of the fight/flight Stress Response that I found to be correct, for me personally, were:
- Fight : angry outbursts / anti-social behaviour
- Flight : anxiety / dissociation / derealization
- Fawn : codependency
- Freeze : depression

I was going to share case studies and examples to show you how this works in action and how addiction is a reasonable, rational response to being triggered as well.
I don’t, however, want to over complicate things.
And, in all honesty, I’m tired of the project now.
This is more than enough, with the history in Chapter 2, to give people information on why they may want to focus on trauma recovery before they believe they have some kind of “disorder”.
I’m going to keep it simple, again, and show you something before I end this chapter (and book!). I’ll then leave this good fight to those with more youth, health and energy.
Because you sure do need those for this one.
I’m also physically unwell and need to streamline for health reasons now. My current challenges are largely due to the fact that some highly respected professionals were unable to see what was right in front of them and caused far more harm than they did healing in my case.
But this story is not uncommon.
The majority of mental health professionals have been given one book to refer to as “the Bible of psychiatry and psychology” to “diagnose” “patients”, you see.
The Diagnostic Statistical Manual of Mental Disorders.
Developed off the back of a hospital administrative manual that was never meant to be a guide to treating people.
With a biological perspective on the causes of mental health conditions that encouraged pretty barbaric and dangerously radical physical interventions as treatments.
Off the back of a government census that relied on census officials, heads of families and slave owners to decide who was or was not sane.
As a variant of WHO’s manual of International Disease Classifications, which was heavily influenced by mental health classifications by the U.S military service of its war veterans.
With the word “reactions” removed in the third revision and replaced with the word “disorders”, by only nine people of mostly one demographic, because (by the leader of the task force’s own admission) “reimbursement from medical insurance would be difficult if the classifications were based on sets of symptoms and were not specific” (to medical conditions).
Which would also protect the personal interests of professionals treating these conditions by making them more affordable to clients.
Which would encourage pharmaceutical medicines as being a first line of treatment.
By a task force of mostly academic psychiatrists who originally had a personal interest in medicalising mental health conditions, as they could not get funding for research because psychology was not considered “scientific” enough to warrant this.
With future task force members having well known and very public ties to the pharmaceutical industry.
No, I am not a “conspiracy theorist”.
All of this is factual, and included in the history of the DSM, available from reliable sources to anyone who is curious enough to ask “how?” and “why?”.
Please feel free to ask questions in the comments. I’ll gladly answer them as best I can and add links for you to access the information I found as time allows.
And please remember that there is (in all probability) nothing “wrong” with you or your children.
Because have a look at this:
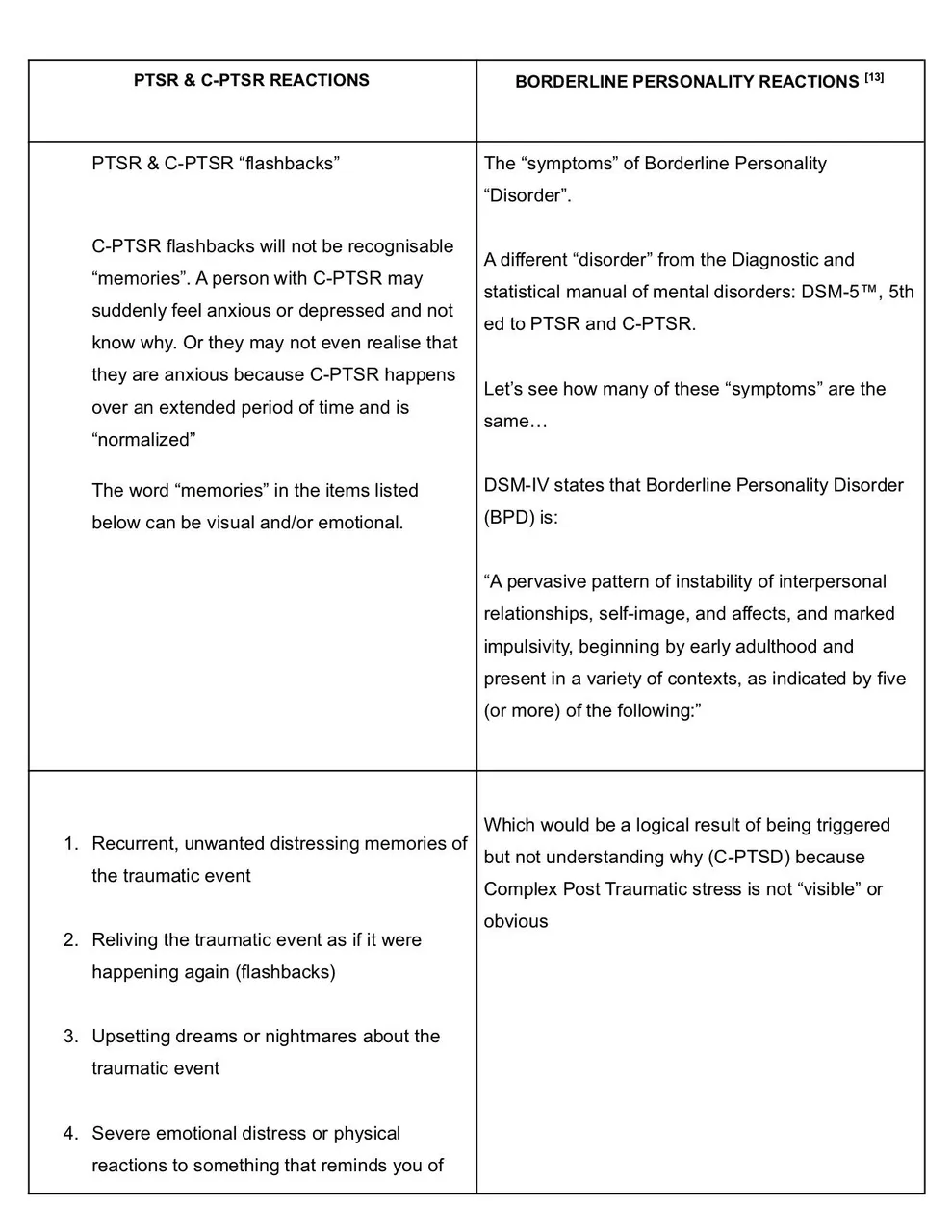
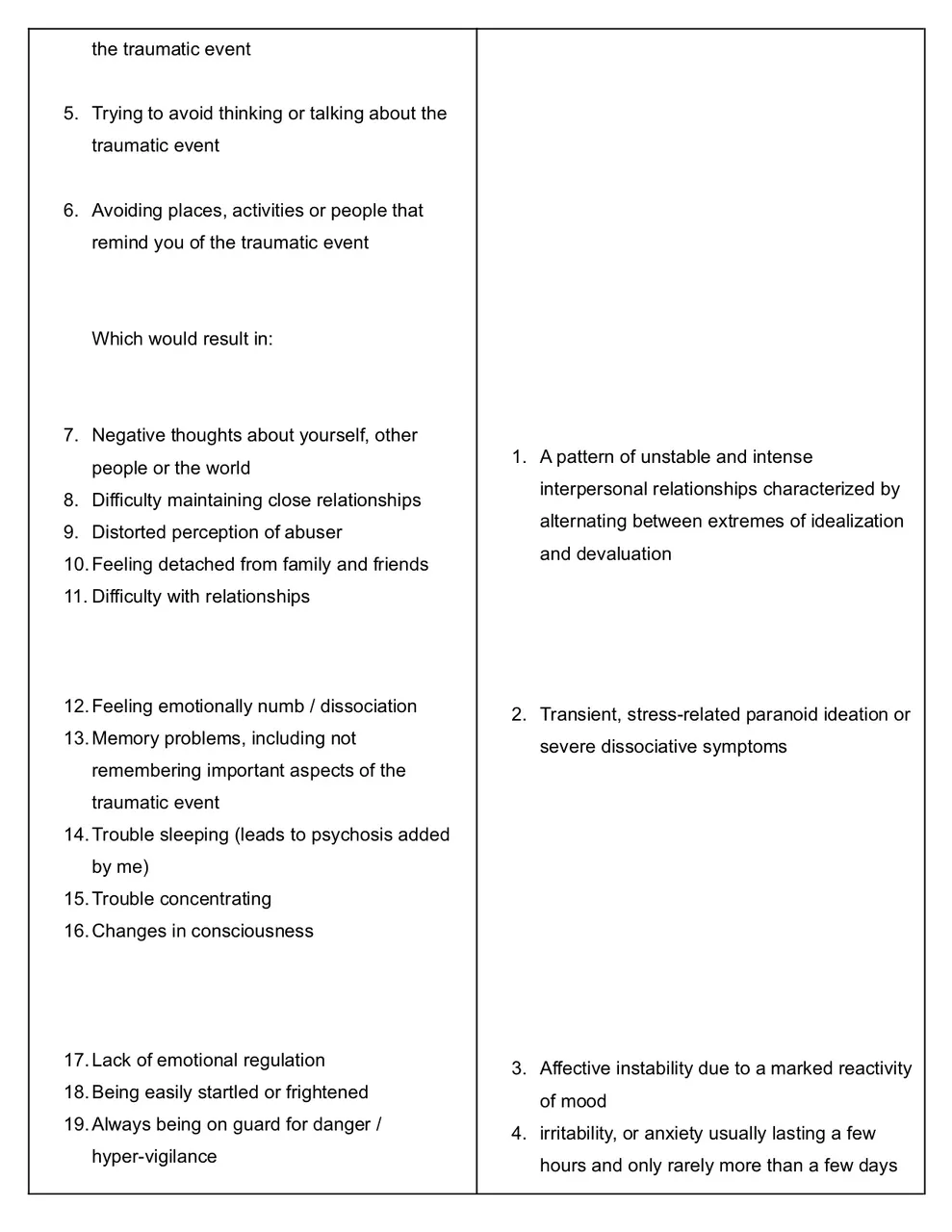
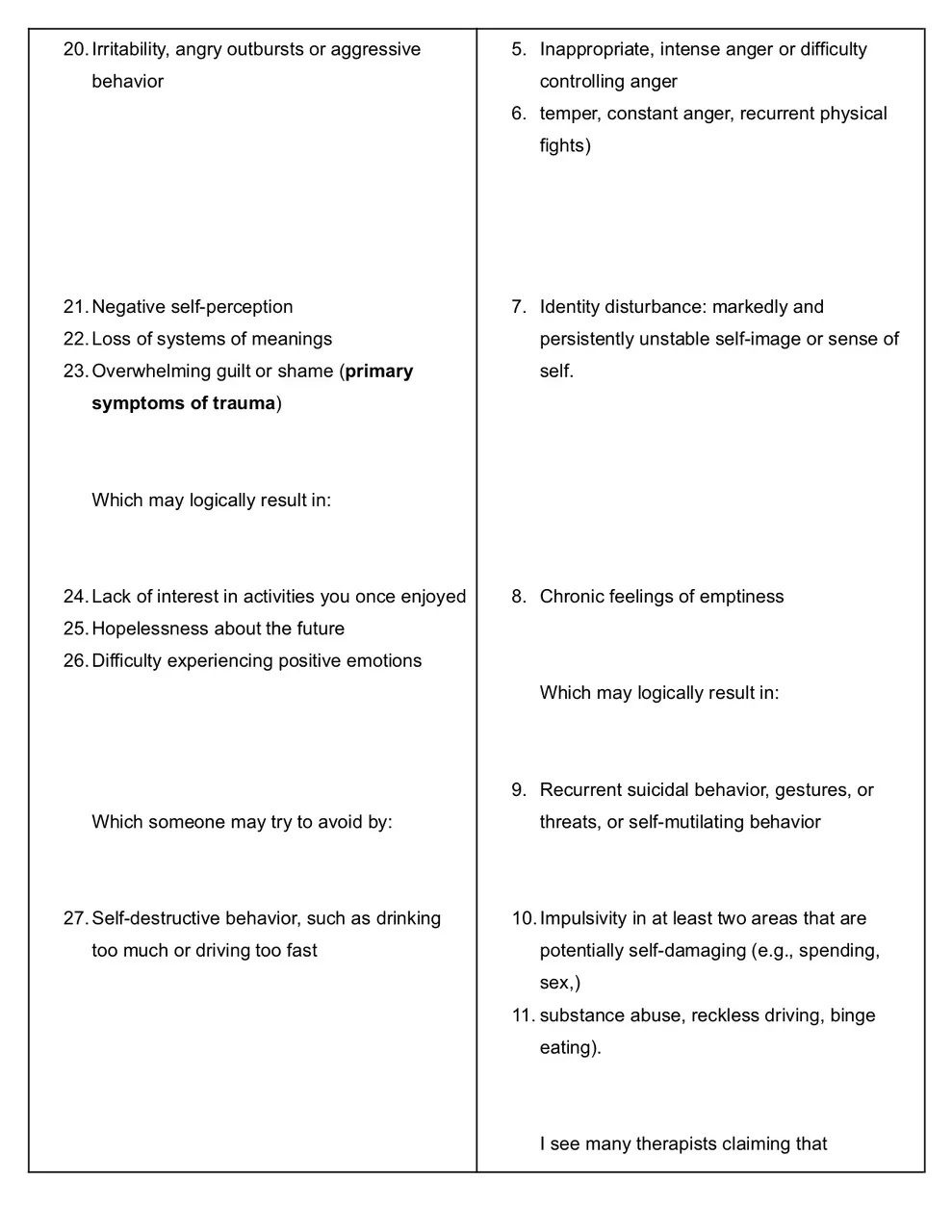

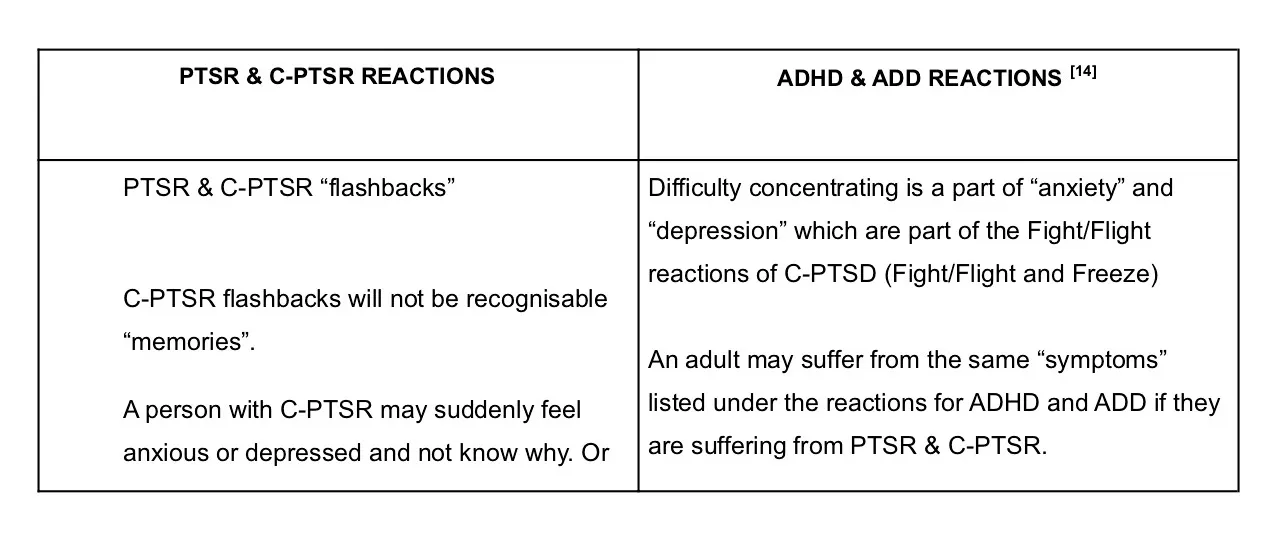
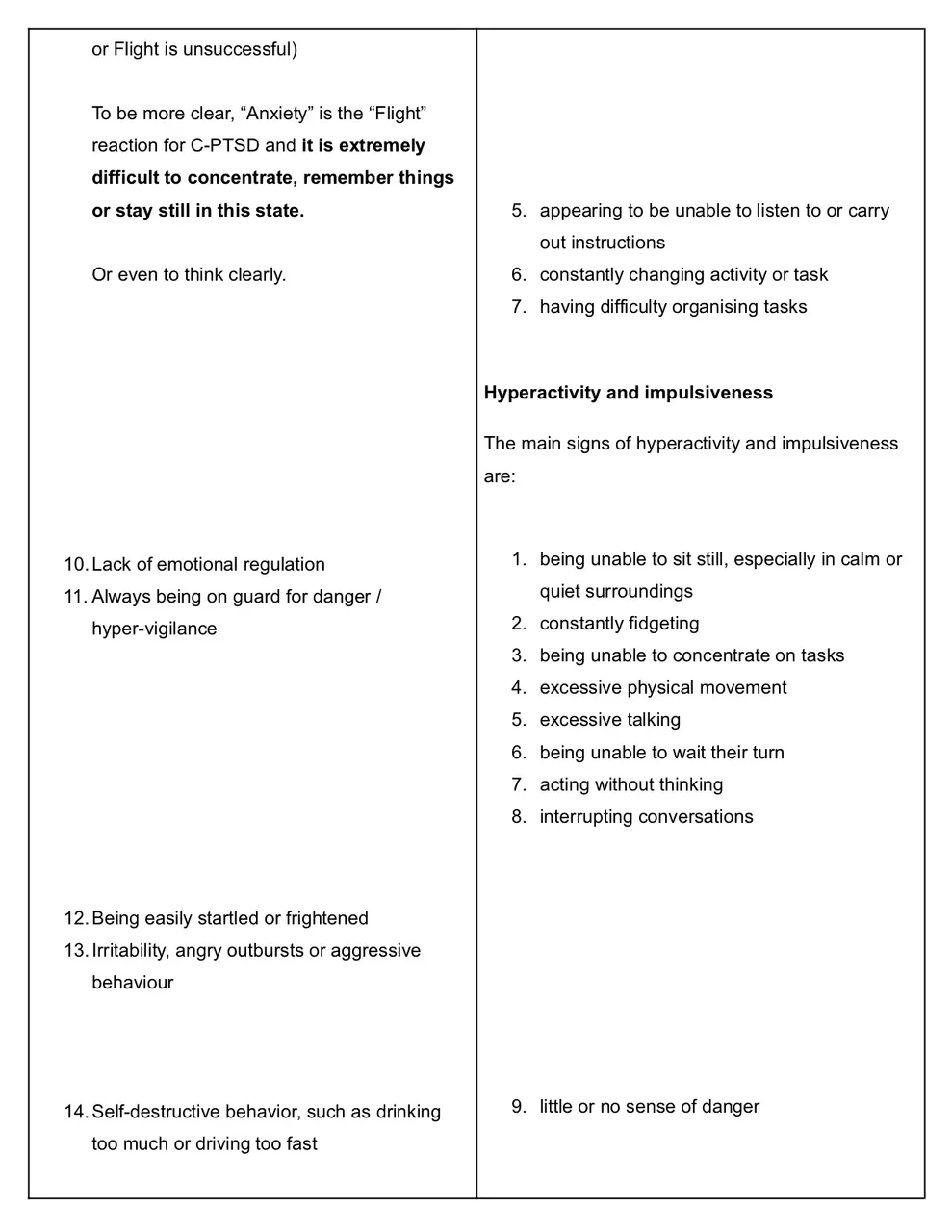

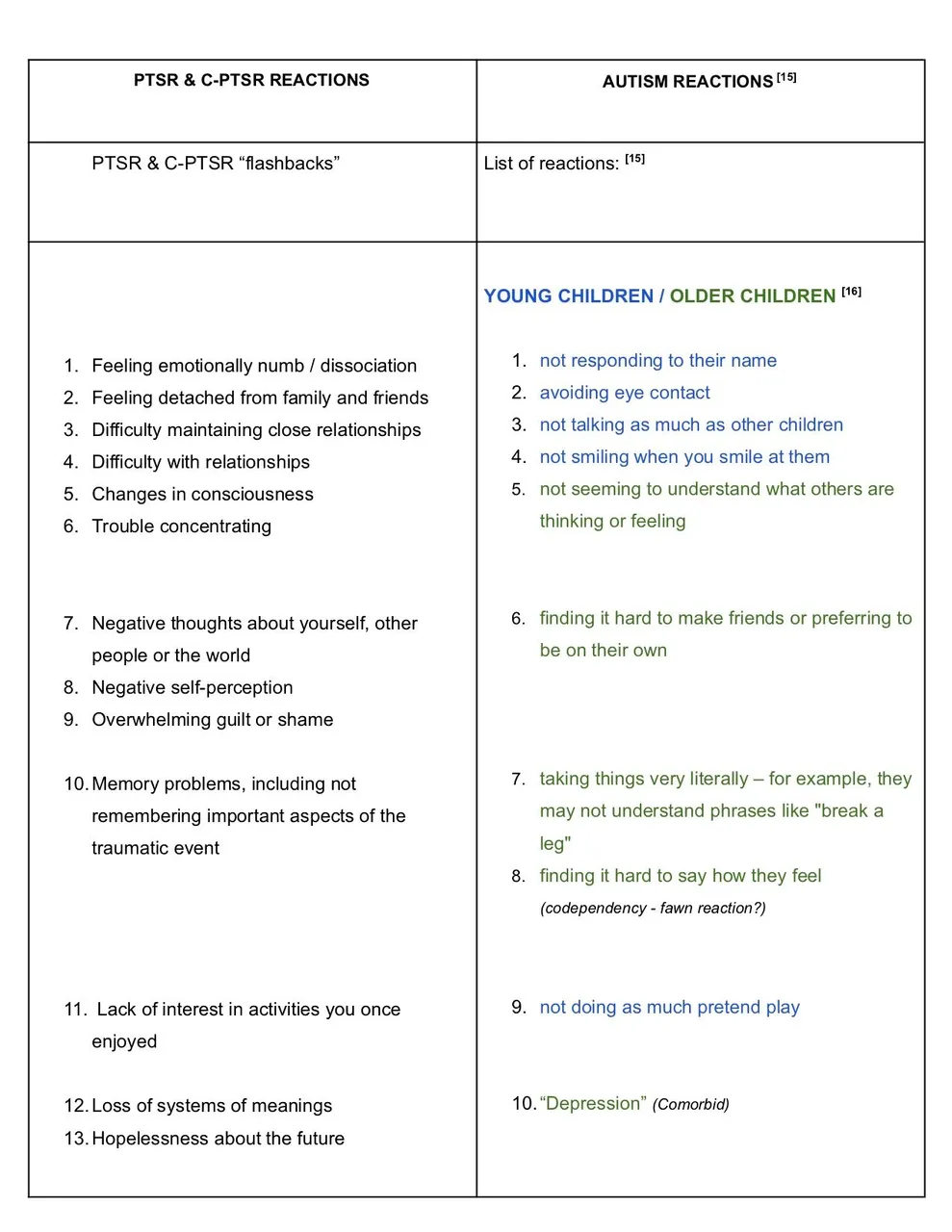
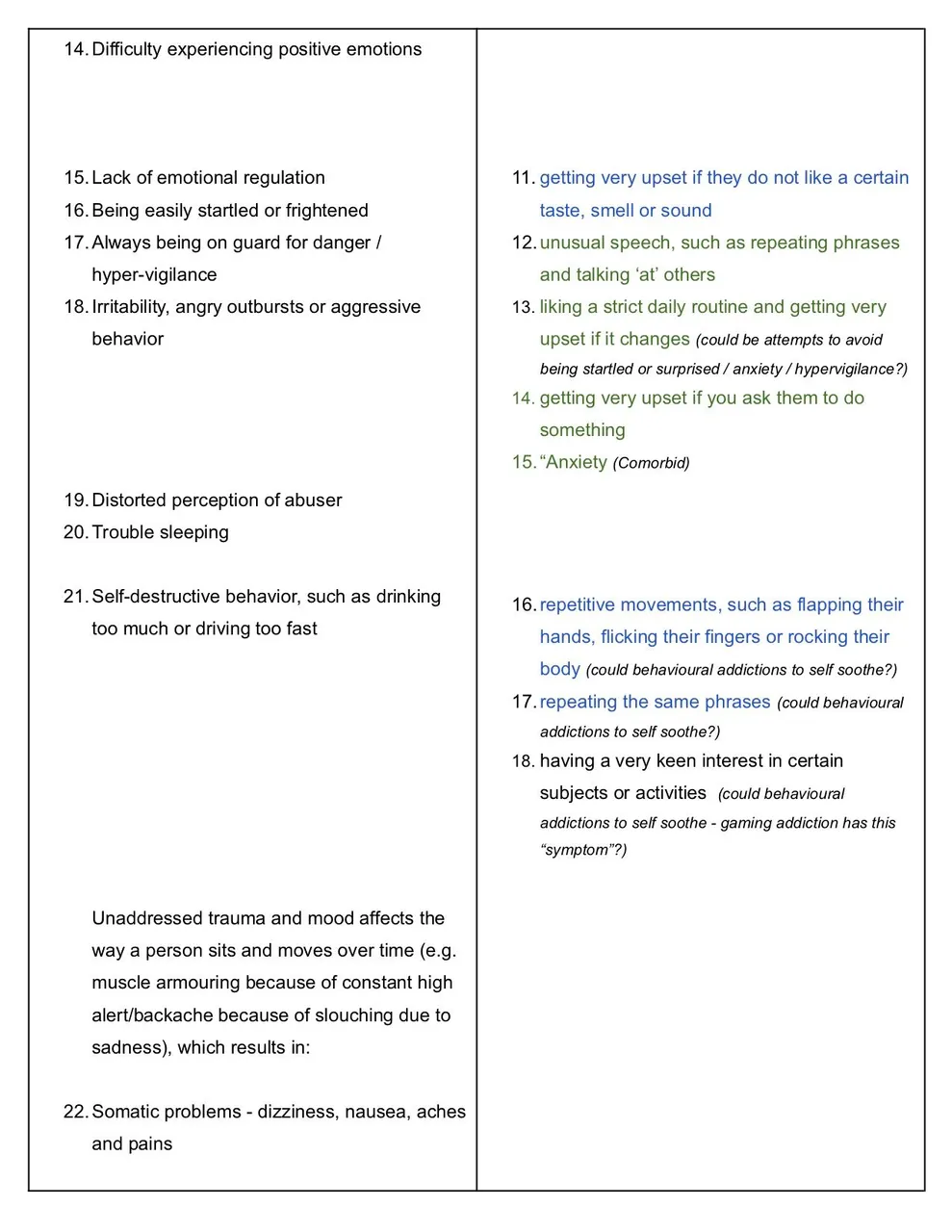

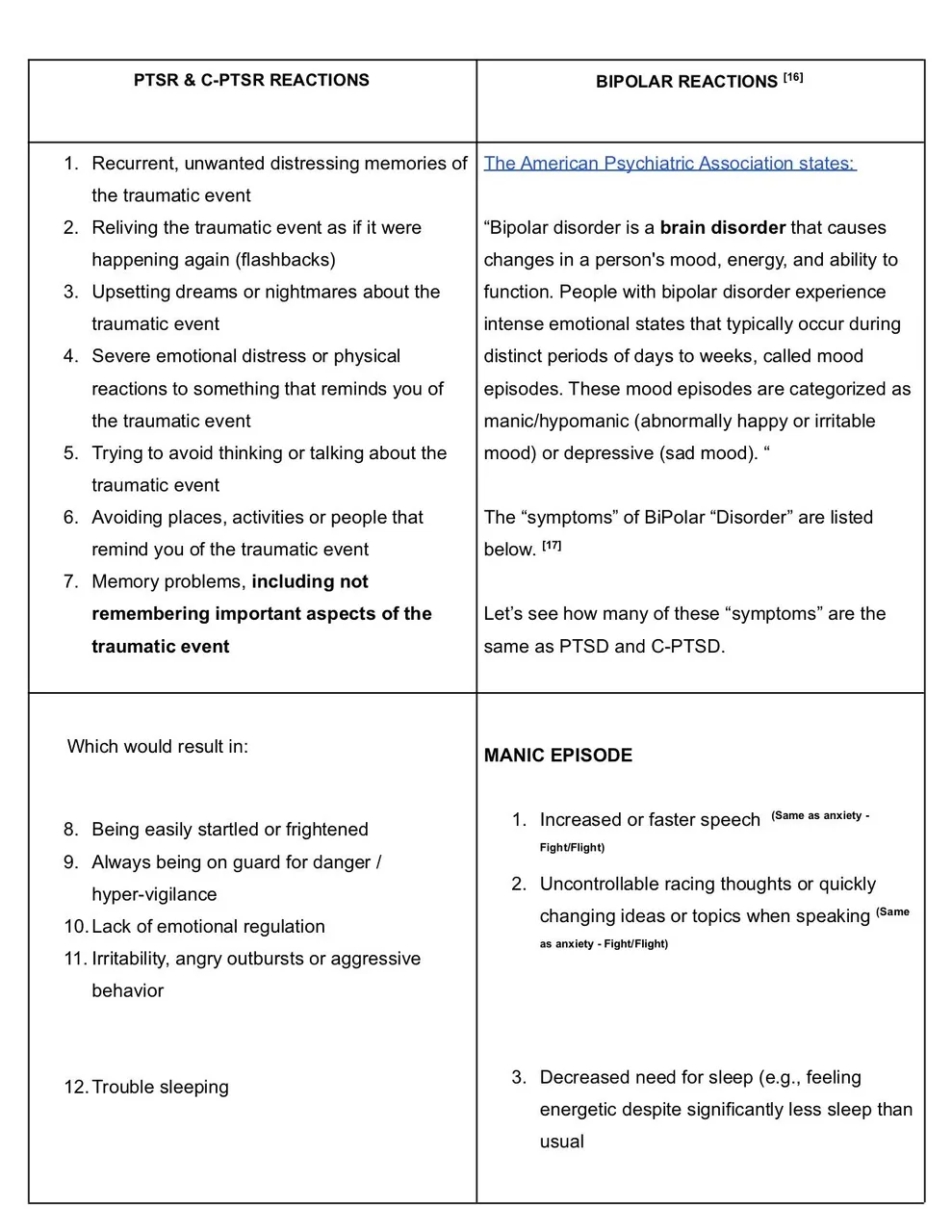
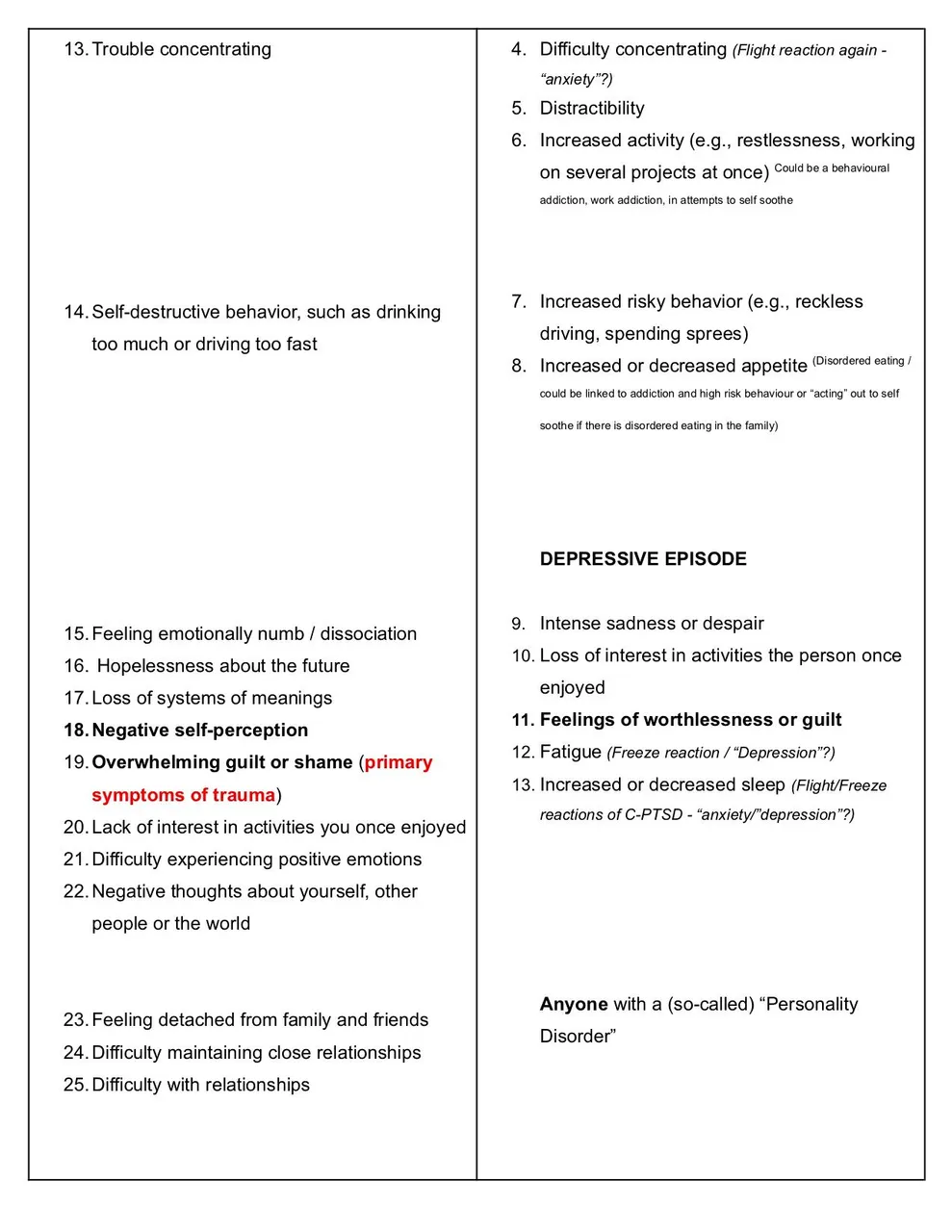

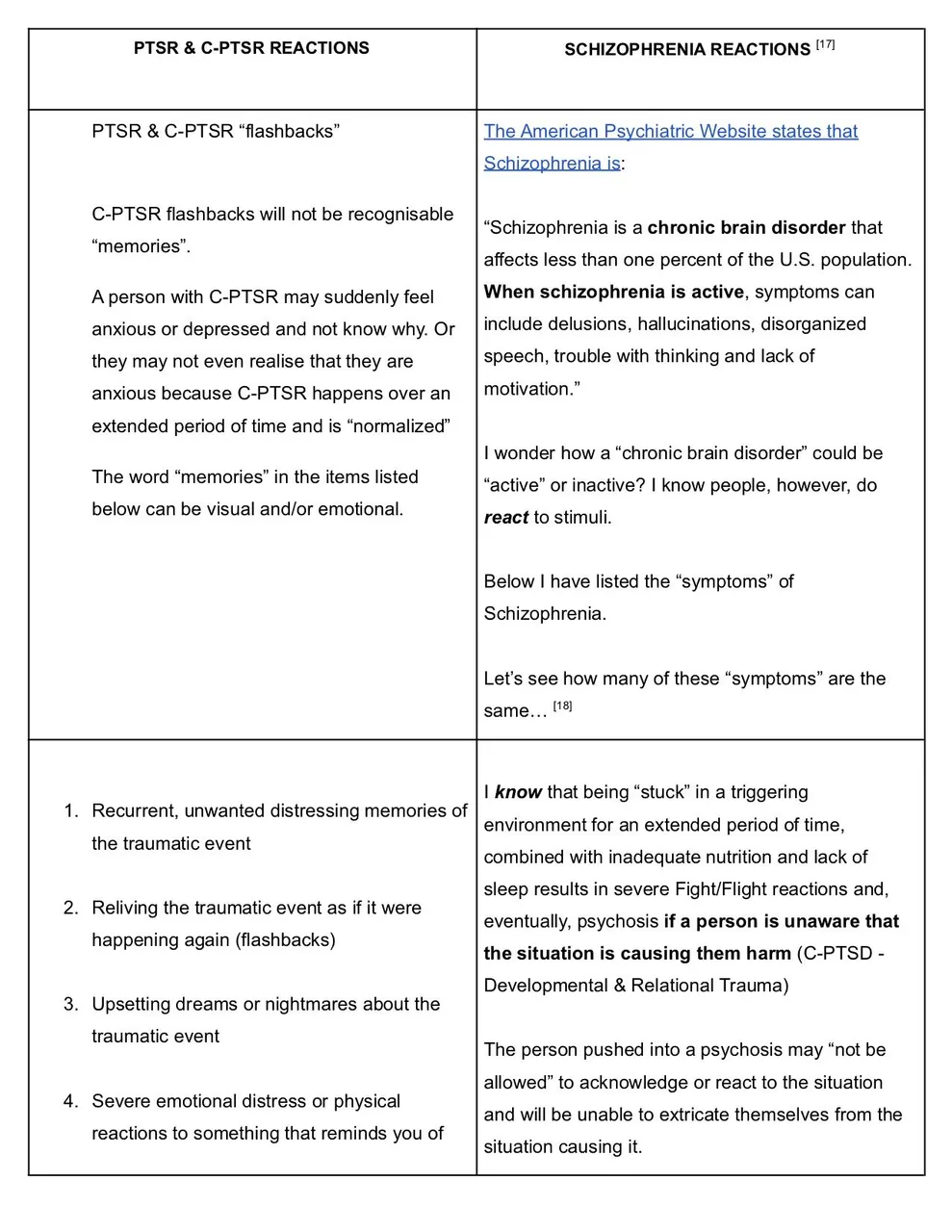
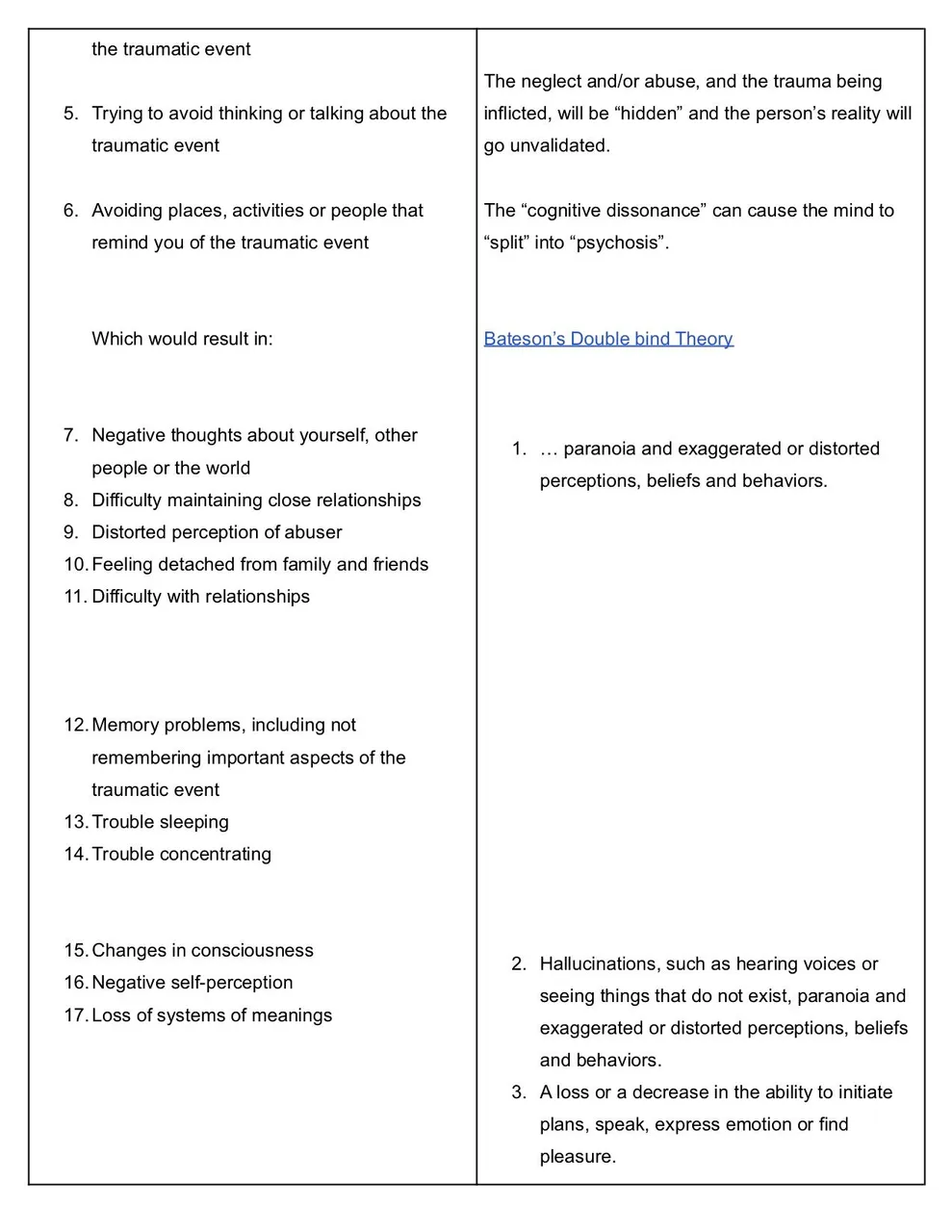

One might apply this formula to any “disorder” listed in the DSM.
All of the “disorders” in the DSM seem to have reactions and behaviours that coincide with, and overlap, each other.
Some of you may think that the “disorders” listed in the DSM don’t have all the reactions of PTSR and C-PTSR, so they can’t be these.
I’d reply that not everyone has all of the symptoms of a real illness, such as influenza, either. And everybody has varying degrees of it, when they do have it, depending on their physical health and environment.
All of these mental health challenges and behaviours may well be the exact same thing, playing out in different ways, dependent on past experiences, current circumstances and environmental triggers. As well as dysfunctional family roles and the resultant behaviours that are adopted accordingly. And the attachment styles of individuals.
If one looks at this from the perspective that a human being’s reactions to their environment are rationally motivated by survival, that is.
Survival in the sense that a stress response to a perceived threat in an environment will kick off the Fight/Flight mechanism.
And this will naturally result in an inability to focus, to remember things, to concentrate, to engage socially or even to sit still at times. And may cause individuals to act out in unusual and anti-social ways.
If the person is unable to fight or flee, the stress reaction may then move into fawn or freeze (depression). Mentioned way back in the 50’s by doctors who already knew best!
"The description for the category of Psychoneurotic reactions in the DSM-I read:"
"The chief characteristic of these disorders is “anxiety” which may be directly felt and expressed or which may be unconsciously and automatically controlled by the utilization of various psychological defense mechanisms (depression, conversion, displacement, etc.) (DSM-I, American Psychiatric Association, 1950)
…“Anxiety” in psychoneurotic disorders is a danger signal felt and perceived by the conscious portion of the personality… (DSM-I, American Psychiatric Association, 1950).
It is produced by a threat from within the personality (e.g., by supercharged repressed emotions [my boldface], including such aggressive impulses as hostility and resentment), with or without stimulation from such external situations as loss of love, loss of prestige, or threat of injury.” (DSM-I, American Psychiatric Association, 1950)
Doctors around the 50’s already knew what they should be treating to successfully help people with mental health challenges.
And addictions may simply be behaviours that are adopted in attempts to self soothe and find safety. Learned coping mechanisms from the family dysfunction, from primary caregivers, by rote.
As mine were.
Addictions should never, in my experience, have been considered “disorders” or some kind of “disease” in and of themselves.
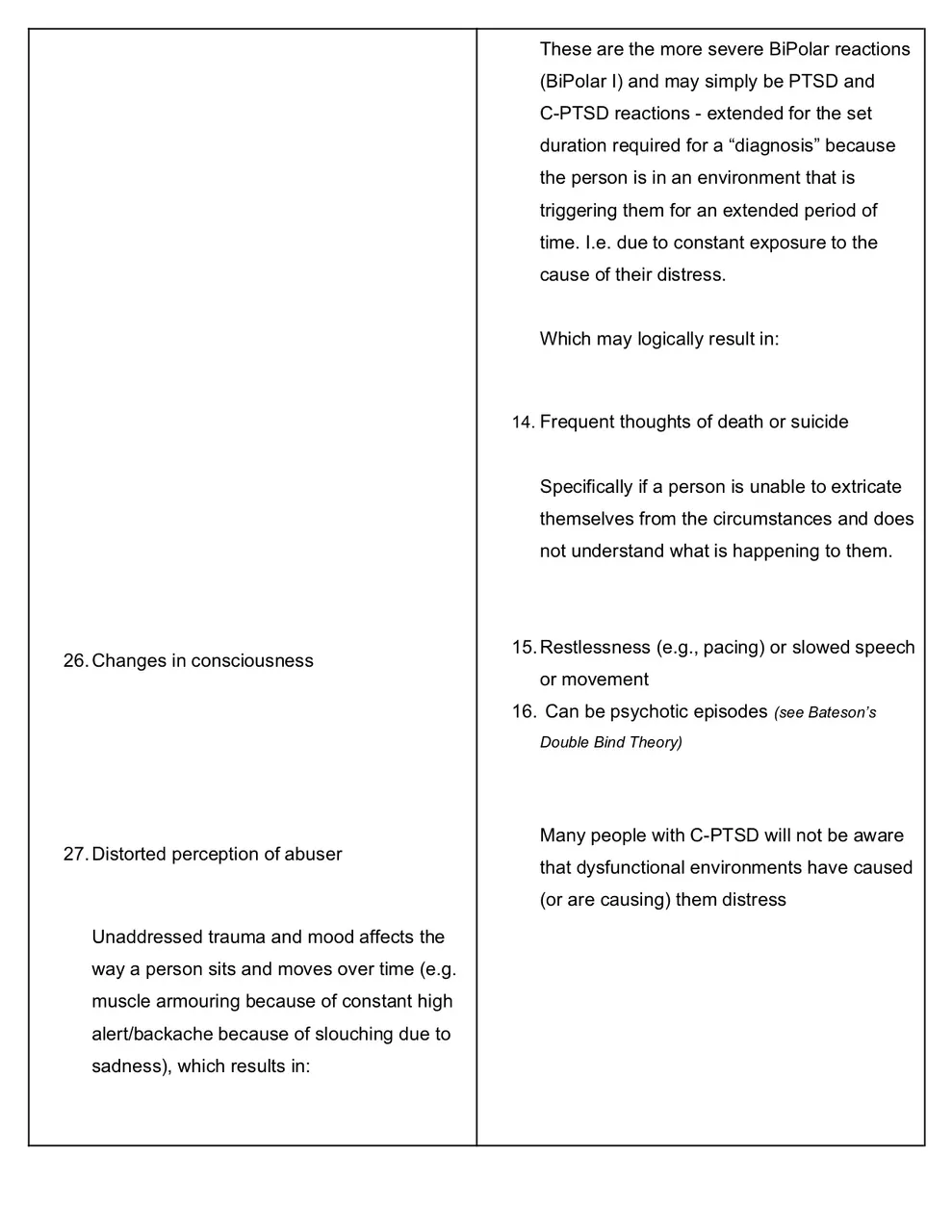
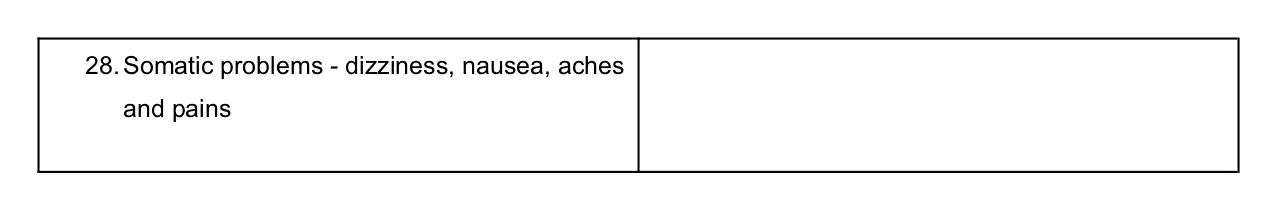
The more serious categories of reactions, such as BiPolar and Schizophrenia, were much the same for me. Only far more intense because I was still in an environment that was a threat to me emotionally and psychologically even though I wasn’t fully conscious of this.
The cognitive dissonance between my “instinct” (the Amygdala) and my learned social dynamics eventually drove me into a psychosis.
Gregory Bateson has written a paper on this called “The Double Bind Theory”.
His theory explains exactly what my psychosis was.
By the time I took myself in to see a medical professional, in my late twenties, I was having full blown auditory hallucinations, was pretty delusional and I could barely leave my home. My reactions were that severe.
This was due to ongoing exposure to a major trigger, from a primary trauma, in an environment from which I was unable to extricate myself. I was also being told nothing was happening and I was imagining things. i.e. my “reality” was not being validated.
Interestingly enough, this almost happened again in my late forties…
when I was back in the exact same situation with the same triggers for an extended period of time. And my reality was not being validated again.
This was my biggest clue as to what some of my mental health challenges actually were.
Environment is crucial when one is looking at lasting recovery for mental health and addiction.
If we are looking at psychosis from the perspective of Bateson's theory and the great forerunners of psychoanalysis as well.
The mind eventually “splits” in order to avoid the “truth” of some situations and “delusions” or “hallucinations” are the unconscious trying to bring things to light in a lateral, and therefore less threatening, way.
In this way, the person may be able to acknowledge the situation more "safely". Yet another attempt, by the unconscious, to encourage the person to take action in order to move them into safety and/or heal them.
In order to survive.

The DSM offers guidelines on the duration of these reactions being present, in order for a “diagnosis” to be made. Various reactions for various “disorders” must be present for a set duration of time in order for them to be considered a “disorder”.
But if a person is permanently in an environment that the reptile brain perceives to be a threat, this may be the reason that some people’s reactions are ongoing. Or go as far as a psychosis.
It may all be far more simple than we’ve been led to believe it is.
Because medical insurance companies will not pay out for things that are not classified medical illnesses. Which is exactly why the word “disorder” was added to the Diagnostic and Statistical Manual of Mental Disorders in the third revision in the 1980’s. By the admission of the leader of the task force, Dr Robert Spitzer, himself.
What a sad state of affairs we find ourselves in when, it seems, the early psychiatrists and psychologists had already found the correct treatment for these challenges way back in the 1950s.

Current practice and treatment failings
- Current standard practice of diagnosing people with incurable chronic medical “disorders” prevents recovery.
- Current practice further traumatises individuals due to lack of validation, social stigma and further isolating them (which causes trauma) by labeling them as “disordered”, “diseased” or “ill” because of their thoughts, feelings and reactions.
- Validation of an individual’s experience is, arguably, the single most vital component in trauma recovery (as is trust in the professional guiding it).
- Current practice does not address the underlying cause of the reactions.
- Prescribing pharmaceutical medications for “disorders” for lifetimes, often with unpleasant side effects which require even more medications, only alleviates the symptoms of the underlying causes and prevents proper recovery.
- Telling an “addict” or a “mentally ill” person (in treatment and support groups, no less) that they are “diseased” or “disordered” and need to make amends to, or read letters of consequences from other family members who are a part of and also responsible for the family dysfunction, in a public group setting, is emotionally and psychologically abusive.
- In dysfunctional families and the roles assigned, there will usually be a “scapegoat” or “identified patient” in the family who is unconsciously assigned the role of carrying the family “insanity” (trauma) and dysfunction (denial). Denying family dysfunction and blaming one individual is “gaslighting” and is, again, listed as emotional and psychological abuse.
- Blaming one individual also assists the dysfunctional system in keeping the trauma buried through denial and by avoiding accountability. This will prevent recovery for both the individual and the system itself. And probably traumatize future generations through hereditary and multi-generational trauma.
- The same issue applies to families/people who are suffering and society at large. By stigmatizing these challenges as “diseases” and “disorders” blame is apportioned to the individual or family and not the failings and stressors of a society.
- One 45 minute session is not adequate for a proper background history or any kind of authentic psychoanalytic process. Yet people are now being diagnosed with disorders and prescribed chronic psychiatric medication for life times as standard practice in the first 45 minute session with professionals.
- Three weeks is not enough time to help anyone “recover” from an addiction or mental health crisis. But three weeks of treatment is all medical insurance will cover and pharmaceutical medications are the fastest way to stabilize people, resulting in an overprescription of medications.
- Psychology and psychiatry are not hard science or medicine. They are opinion.
What seems “normal” to one person in one country may seem abnormal to another person from another country, culture, gender, age group, ethnic group.
Yet, worldwide, we now believe we, or our loved ones, are sane or “disordered”/insane because of the opinion of one small demographic from one country in the world.
That is fucking insane! (Sorry, Alan…a sweary word sneaked in while you were away)
My apologies if this isn’t as professional and succinct as I’d like it to be, by the way. The editor on this project fell ill (properly physically ill) and had to step back.
And I’m not a medical doctor or a psychologist.
I’m just a Schizophrenic, BiPolar, Borderline, Anxiety & Depression Disordered Addict who is, somehow sitting writing this today, four years medication free with no further treatment necessary.

Free to share and distribute
With thanks to the community on Hive for your courage and open-mindedness.
This project would never have been completed without your incredible engagement and support.

Citations
[9] APA Dictionary of Psychology. (n.d.). Retrieved February 16, 2023, from https://dictionary.apa.org/
[10] Post-traumatic stress disorder (PTSD) - Symptoms and causes. (2022, December 13). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967
[11] Gilles, G. (2018, January 26). Understanding complex post-traumatic stress disorder. Healthline Media. https://www.healthline.com/health/cptsd#symptoms
[12] What is Psychological Abuse of a Child? (n.d.). HealthyPlace. Retrieved February 15, 2023, from https://www.healthyplace.com/abuse/child-psychological-abuse/what-is-psychological-abuse-of-a-child
[13] Carey, E. (2018, May 30). Child emotional and psychological abuse. Healthline Media. https://www.healthline.com/health/child-neglect-and-psychological-abuse
[14] Borderline personality disorder - DSM -5 and ICD -11 diagnostic criteria. (2021, December 14). Psych Scene Hub. https://psychscenehub.com/psychpedia/borderline-personality-disorder-dsm-5-and-icd-11-diagnostic-criteria/
[15] website, N. (n.d.-a). Signs of autism in children. Nhs.Uk. Retrieved February 16, 2023, from https://www.nhs.uk/conditions/autism/signs/children/
[16] What are bipolar disorders? (n.d.). What Are Bipolar Disorders? Retrieved February 16, 2023, from
https://www.psychiatry.org/patients-families/bipolar-disorders/what-are-bipolar-disorders
[17] What is Schizophrenia? (n.d.). What Is Schizophrenia? Retrieved February 16, 2023, from
https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia
References
- Gupta, S. (2022, June 21). What is psychological abuse? Verywell Mind. https://www.verywellmind.com/psychological-abuse-types-impact-and-coping-strategies-5323175
- NSPCC. (n.d.). Emotional abuse. NSPCC. Retrieved February 15, 2023, from https://www.nspcc.org.uk/what-is-child-abuse/types-of-abuse/emotional-abuse/#what)
- Post-traumatic stress disorder (PTSD) - Symptoms and causes. (2022, December 13). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967
- website, N. (n.d.). Signs of autism in children. Nhs.Uk. Retrieved February 16, 2023, from https://www.nhs.uk/conditions/autism/signs/children/

I do not endorse the information shared in K.I.S.S - Keep it Simple Sweetheart Perfect to be used in place of professional medical advice, support groups or specific therapies.
Please do not come off any prescribed medication without the guidance and support of a trained professional.
Please do not step away from any programs of treatment or support groups without the guidance and support of a trained professional.



Edited with GIMP
Please consider adding the developer as a beneficiary for his ongoing work if you use an Arty Bot artwork. At this point it's unnecessary to use repetitive stock images. The only limit is your imagination.
Let's support members of our community first.
A snippet of a voice-note, randomly recorded during a walk in April 2022, on the content I've been trying to share in:
Perfect: An alternative perspective on mental health and addiction
A spontaneous voice-note ended up being, pretty much, the whole book!

The full version will be released on ThreeSpeak when the time is right. Until then, you can read the final chapter of Perfect, "But I Don't Have Trauma" if you're curious to know more about how this works.
The chapter on trauma is too long for a description here on ThreeSpeak, so if you're interested in reading more about how trauma "works" and why you (or your kids) may have it even if you aren't aware of it yet...
please head over to PeakD or Ecency to read the full post.
Chapter 3 is the final part of the book and this project is now complete.

I'm busy ticking boxes and streamlining so that I can focus on my health and some necessary life admin now. I'll answer questions in the comments but please be patient as I'll be offline in patches to do the above. It's time!
I will always respond, though.
Eight or nine years of work on this particular project.
I've lost count...
I can't quite believe it's finally done! 😁
I hope it helps some people.
Keep on keeping on.
Recovery is possible ❤️

Free to share and distribute.
With thanks to the community on Hive for your courage and open-mindedness and to Internet Archive for your service. This project would never have been completed without your resources and support.

I do not endorse the information shared in K.I.S.S - Keep it Simple Sweetheart Perfect to be used in place of professional medical advice, support groups or specific therapies.
Please do not come off any prescribed medication without the guidance and support of a trained professional.
Please do not step away from any programs of treatment or support groups without the guidance and support of a trained professional.

Edited with GIMP
Video made with Blender.org
Please consider adding the developer as a beneficiary for his ongoing work if you use an Arty Bot artwork. At this point it's unnecessary to use repetitive stock images. The only limit is your imagination.
Let's support members of our community first.
▶️ 3Speak
